Does ABA cause PTSD?
The answer is no, ABA Therapy does not cause PTSD. One of my followers explained where the rumor originated from. There was only one survey about the subject and it was published in a pay-to-publish journal.
The idea that ABA causes post-traumatic stress disorder (PTSD) stems from one online survey that was circulated amongst social media groups (Kupferstein, 2018). The survey included 217 respondents who were caregivers of children with autism and 243 respondents who were adults (18-73 years of age). The adult respondents identified themselves as autistic, with or without a clinical diagnosis of autism; their average age at the time of their autism identification was over 25 years of age. The survey included questions about post-traumatic stress symptoms (PTSS); it did not ask for an independently verified confirmation of a diagnosis of PTSD. The survey also did not define ABA-based interventions, apart from stating that these were “early interventions”.
In addition, no actual numbers are reported in the paper, just the percentage of respondents. A quick calculation illustrates a problem. Given that the non-completion rate of the survey was high (only 50% of adult respondents and 61% of caregivers answered all of the survey questions), this means that only about 120 adults with autism and about 130 caregivers completed the survey fully. Of the adult respondents, 11% are reported to have experienced ABA-based interventions, which means that only 11 or 12 adult respondents had experienced some kind of ABA-based interventions.
As mentioned above, though, there are inconsistencies because ABA-based interventions purportedly were experienced in early childhood, but autism was not diagnosed until these adults were over 25 years of age. It is very unlikely that someone would have been given early ABA-based autism interventions unless they were diagnosed with autism at an early age. In any case, of the adult respondents who said that they had experienced ABA-based interventions, 62% reported some PTS symptoms. In other words, this appears to apply to a total of 6 or 7 adult respondents to the survey, clearly not enough to draw definitive causative conclusions about a whole population or a science.
Apart from drawing on very low numbers and unconfirmed diagnoses, there is no mention in the paper of any additional or multiple traumatic life-events during adulthood, such as bereavement, abuse, accidents, or near-death experiences, that have been linked to post-traumatic symptoms (Grabrucker, 2013; Sharain et al., 2009). Furthermore, Kupferstein also asserts that mothers who were exposed to childhood trauma, including physical, emotional, or sexual abuse are nearly twice as likely to give birth to a child with autism. Recognition that childhood trauma may be caused by parental trauma is evidenced in research related to transgenerational transmission of parental trauma and/or trauma-affected parenting (Fargas & Dillenburger, 2016).
Kupferstein (2018) compromises her own conclusions with the statement that “[a]utistic people have a sensitivity to the way any situation is initially appraised, and a benign situation which was perceived as harmful or threatening to the individual can become a PTE [potentially traumatic event] which could trigger PTSS due to their underlying vulnerability” (p.20). Clearly, then, even if these adults experienced helpful and “benign” interventions, the vulnerability, sensitivity, and sensory over-selectivity that is part of the diagnosis (APA, 2013) could have led to PTS symptoms.
There are many other severe methodological problems with this study that were exposed some time ago and for these reasons, the study itself has been discredited. “Kupferstein’s results should be viewed with extreme caution due to several methodological and conceptual flaws including, but not limited to, leading questions used within a non-validated survey, failure to confirm the diagnosis, and incomplete description of interventions.” (Leaf, Ross, Cihon, & Weiss, 2018, p122). Yet, the myth that interventions that are based on the scientific application of behavioral principles cause PTSD remains and is cited frequently in tribunals. In reality, there is much more evidence that people with a confirmed diagnosis of PTSD seek and are supported by effective and evidence-based behavior analytic procedures, such as behavioral activation, graded exposure (Gros et al., 2012), and cognitive behavior therapy (NICE, 2017).
Read more about it here
ABA Therapy does not cause PTSD or trauma.
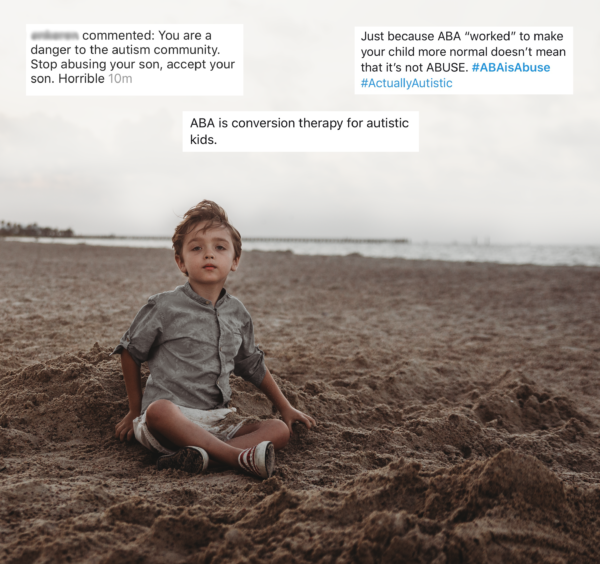
ABA therapy is not abusive. It’s not ableist, nor is it conversion therapy, either.
Our autistic children don’t do ABA therapy from some misplaced parental desire to make them “normal”, and nor is it to eliminate their autism. They’re in therapy because they need to learn the essential skills to keep them safe, happy, and independent, and to not make an earnest attempt at this would be wrong.
Our children are in therapy to learn that running in front of cars is dangerous. So they can learn to communicate, through their own voice or through the speakers on a tablet. So they can get dressed by themselves. To tolerate eating the foods they need to be healthy. And to use the bathroom in a sanitary and dignified way of which everyone is worthy.
Autism is a broad spectrum, so while many higher-functioning autistics can navigate society without much help, there are many others, like my son, who need substantial support for the most basic everyday functions. In addition to lovingly helping them, to — in the name of neurodiversity — not help them learn to help themselves would be nothing short of negligent and cruel.
I’m not ready to accept that almost all of Charlie’s thoughts and feelings may forever be trapped lonely in his mind, frustrating him and isolating him from the world. A translation could exist — therapy for Charlie means professionals working full-time to access it.
I’m not ready to accept that he’ll never have a sense of danger, that every moment of his life outside the home will require holding hands.
And I am not ready to accept that Charlie may never be independent enough to use the bathroom with the dignity befitting any and all humans.
So, until there’s not an ounce of hope left in me — until forever — our family will work with Charlie to work *for* Charlie, whether that’s ABA therapy or whichever type of help will help.
If in your eyes, that makes me an abusive mother, I don’t need to know what a good mom is.
You can read my balanced view on ABA therapy as an autistic adult here.
Does ABA Therapy cause PTSD? One last time, NO.




9 Comments
Diane
2020-07-17 at 8:23 PMHey, Eileen!
I found your blog after browsing through Google. I love what you’re posting, especially this article on ABA therapy not being abusive.
I actually created a resource for your text “aba therapy”, which is a link to a free aba resource and progamme which might be interesting for your readers if they’re looking for further information on this topic.
Would you want for me to send it over?
I hope you have a great day,
Thank you,
Diane
x
2020-09-21 at 2:31 AMLMAO, You clearly have never actually listened to autistic people about why ABA is bad. The things you say you want for your son can all be achieved just fine through therapy that ISN’T ABA, and won’t leave your child struggling with trauma when he’s older.
Kelsey Goodwin
2021-08-07 at 6:32 PMShe’s autistic but good try! I’m sorry you are uneducated about the topic! Sending my love to you sweetheart
Naughty Autie
2024-01-06 at 6:20 PMThere’s no evidence that Eileen Lamb is autistic, and I’m not even demanding that she show a diagnostic report. I just want her to start showing just a modicum of the empathy and theory of mind that are heightened in actually autistic people.
David N. Andrews M. Ed., C. P. S. E.
2021-09-05 at 2:29 AMUm … you’re not very well informed on ABA, are you? You think you are, sure; but you haven’t actually studied it – like, ABA itself – have you?
Applied behaviour analysis is not and never has been therapy: it is the applied/real-world branch of behaviour analysis. The other two branches are:
a- the experimental analysis of behaviour (the branch concerned with uncovering the fundamental principles of how behaviour actually works), and
b- radical behaviourism (the scientific philosophy behind it, ‘radical’ in the sense that it is thorough-going – very rigorously scientific, without recourse to explanatory fictions).
The aim in applied behaviour analysis is to assess the validity of claims about the teaching methods used in facilitating the acquisition, development and maintenance of skills. This is an applied research definition of ABA. Practitioner ABA is not different except in that data is collected from one participant only: the person being taught the skills. Instead of using statistical and experimental methods used in research conducted with participant groups, practitioners use specific experiment designs that are appropriate for studies with a sample size of one, such as reversal designs (in which a baseline measure of skill completion is taken and then, after skill teaching has taken place, the measure is repeated in the same way so as to maintain data reliability).
The teaching is done following the learner’s lead: it is rooted in B. F. Skinner’s work on operant learning – in which the learner engages in an action and, if it is even the slightest bit like the skill being taught, this engagement in action/skill-use is reinforced positively. This means that an appetitive stimulus is presented, based on what is determined in a reinforcement assessment conducted previously. Initial trials are intensively reinforcement-heavy until the learner has achieved a reasonable degree fluency in the use of the skill(s) being taught. These skills are then reinforced more sporadically, in order to maintain skill use.
Anyone who has undergone teacher training will notice that this is exactly what teaching is – presentation of a contrived situation in which a skill must be used in order to solve a problem. The difference here is that the collection of data is more rigorous than that seen in teaching. This is because, given the n = 1 sample size, more data is needed in order to determine whether the teaching is what caused any measured increase in skill fluency/competence. The analyst is checking the validity of claims made regarding the usefulness of a method for a specific learner. This immediately diffuses charges that practitioner ABA is ‘one-size-fits-all’: clearly, given the fact that a given method may work brilliantly with learner A but will tank when used with learner B, it is imperative that the best available teaching method for that specific learner is used so that said learner has the best possible chance of learning that skill.
And that is what ABA is at its core.
In 1968, Baer, Wolf & Risley wrote up a very specific definition of what applied behaviour analysis is. They took a dimensional approach; it is:
applied – focussing on socially-significant skills;
behavioural – concerned with teaching people how to do something effectively;
analytic – that is, can demonstrate the effectiveness of teaching with analysed data that shows what part of the teaching was responsible for increases in competence/fluency in the use of a given skill;
technological – in that it can be described in such a way that another person can repeat the teaching process with another person (using the best available teaching method for that person!) and achieve a similar level of effectiveness in the teaching process;
conceptually systematic – in that the methods used in teaching are maximally grounded in behavioural principles as delineated by Skinner and his colleagues;
effective – in that the process of teaching brings about a significant change in the fluency/competence of skill use by the learner;
heneral – such that the gains aforementioned can be fostered in a variety of settings rather than just the onebin which it was learned.
Unless an intervention falls entirely within that set of dimensions, it cannot be called ABA. So, not all behavioural interventions are ABA.
I shall break here for sleep. The onus for understanding this information is on you.
David N. Andrews M. Ed., C. P. S. E.
(autistic autism-specialist behaviour-analytic educational psychologist)
Meghan Mengel
2020-12-05 at 2:26 AMI found your site because I have picked apart this issue for years and I have had such a hard time articulating myself the way you have. We have worked so hard to support our son’s learning style, and interests, to love him as he is and meet him where he is and its because of these things that we reached for ABA–Because we want to teach him how to keep himself safe, and how to care for himself. The first thing our therapist taught him was “No” which he was able to communicate non verbally prior to working with her. Now he can back his “No” with an emphatic verbal command for those who may not fully understand him the way we do. I can talk all day long but as a trauma survivor I struggled with not having a voice in this life–along came my son and the last thing I was going to do was have him feel unheard–regardless of language. Its my job to protect him and equip him for life. Thank you for your article it really resonated in my heart.
Faye Taylor
2023-01-17 at 8:45 AMY’all can get fucked!! You obviously haven’t listened to autistic adults on this topic.
Victor
2023-05-13 at 4:48 AMThe author of the blog post is an autistic adult. Pipe down and grow some manners, child.
Sabh
2023-05-29 at 10:05 AMFuck ABA